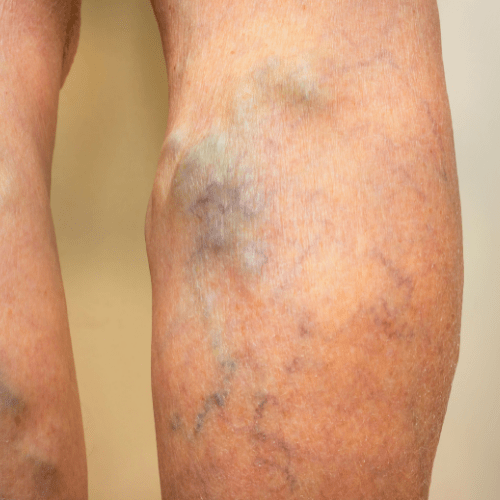
A varicose vein is a condition that manifests in vein deformities ranging from enlarged veins to twisted and purplish-looking veins. Studies by the society for vascular surgery reveal the condition is quite common in America and affects roughly a third of the entire country’s population. Varicose veins can be painful if blood pools around the affected area, causing the build-up of pressure and toxins, which cause an ulcer effect that can be excruciating for the patient.
Though the condition can affect any superficial vein in your body, the blood vessels in your legs are most at risk because walking and standing upright for extended periods put immense pressure on your leg veins. Read on to discover what causes varicose veins, common symptoms as well as prevention and control measures.

Facts about varicose vein
• While common signs of a varicose vein may include bulging, twisting, and dark purple colorations of the leg veins, sometimes the affected veins may lie deep in the flesh, making the condition harder to diagnose. Invisible varicose veins can bring pain and discomfort to the patient for extended periods without knowledge of the underlying condition.
• While pain and discomfort are common symptoms, some patients may not experience other symptoms beyond vein discoloration. For such people, spider veins are merely a cosmetic concern.
• Varicose veins are treatable through self-care for mild cases or medical procedures involving removal and closure of affected veins for severe cases.
What causes vein pain and discomfort?
Arteries supply blood from the heart to the rest of our body organs, while the veins supply deoxygenated blood from the body tissues back to the heart. To facilitate blood return to the heart, the veins in our legs and arms must overcome gravitational pull, a phenomenon made possible by tiny valves.
The valves open to allow blood flow to the heart and close to prevent the backflow of blood. If the valves become weak or damaged, backflow of blood arises, leading to the pooling of blood in the veins. These pools of blood cause the veins to bulge, stretch, and twist, causing pain in the affected region.
Vein valve damage can arise due to various factors ranging from obesity to old age and long periods of sitting, standing, and walking. Sometimes vein pain can occur due to factors related to environmental conditions such as extreme temperatures. Vein-related discomforts can also arise due to bacterial skin infections.
Risk factors associated with varicose veins
Below are factors that can heighten an individual’s risk of developing spider veins.
1. Aging
The likelihood of varicose vein conditions increases as an individual gets older. Over time, the valves in your veins undergo wear and tear, thus affecting blood flow in your legs and feet. Eventually, the valves malfunction aiding the backflow of blood in your veins. Blood collects in pools instead of flowing back to the heart leading to clotting.
2. Gender
Varicose veins are more common in women than men. Women go through hormonal imbalances during their menstrual cycle, during pregnancy, and at the onset of menopause causes relaxation of vein walls. Additionally, birth control pills and hormone-related treatments raise the risk of vein-related complications, leading to varicose veins.
3. Pregnancy
Blood volume increases significantly in a woman’s body during the pregnancy period. Such changes are necessary to facilitate the healthy development of the fetus. However, these changes also cause enlargement of veins in the woman’s legs and feet. During pregnancy, changes in hormone balance can also explain the increased risk of varicose vein conditions among expectant mothers.
4. Obesity
Excessive weight gain puts immense pressure on the heart, arteries, and vein systems. Your body’s blood circulation system has to work extra hard when you put on extra weight. This added pressure leads to enlargement of vein walls and weakening of the valve systems, thus raising the risk of spider veins.
5. Genetic history
If your extended family has a history of varicose veins, then there’s a chance that you might have them too.
6. Lifestyle and nature of work
For some people, their nature of work means they have to spend long hours sitting behind a desk or standing in one position for long hours. Such individuals are at a high risk of suffering from varicose veins being sitting or standing still for long periods interferes with the natural flow of blood.

Symptoms of varicose veins
• Pain and discomfort in the legs is a common symptom.
• Discoloration of the affected vein that may turn blueish or dark purple.
• Fatigue in legs and feet
• Swelling of the vein causes a burning and throbbing sensation.
• Itchiness, discoloration, and hardening of the skin surface around the affected region.
• Cramping of muscles, especially during night times.
The above symptoms become more critical during hot weather or when the individual stands or sits for extended periods. Limited blood flow and swelling of the veins can later worsen, leading to deep vein thrombosis and phlebitis. Thrombophlebitis is caused by inflammation and clotting in the veins. Varicose veins can also pave the way for dermatitis, a condition that causes rashes in the ankles and feet. If scratched or irritated, the rashes burst, causing bleeding and skin ulcers.
Diagnosis and treatment
If the symptoms of varicose veins are mild, self-care treatment procedures are sufficient for suppressing these symptoms. However, without proper care and treatment, mild cases can worsen. Early diagnosis is crucial in dealing with symptoms and preventing further deterioration of the condition.
Consulting a vein physician is the best way to diagnose and treat severe cases of spider veins. Depending on the degree of the problem, the physician can recommend one or a combination of the following treatment procedures:
Compression stockings
• These stockings are designed to suppress swelling of the vein walls, thus lowering the risk of blood clotting. When using compression stockings, doctors advise patients to elevate their legs and massage the leg tissues to aid blood flow in the affected region. Patients may need to wear the stockings for a few months to resolve the vein condition fully.
Surgical treatment
• A physician can recommend surgical procedures if the clotting is severe and the vein function is significantly compromised. Ligation is a standard surgical procedure that entails completely removing the affected vein to stop blood pooling.
Sclerotherapy
• Sclerotherapy entails injecting a sclerosant into the affected vessels to clear the clots in the affected area. The procedure is safe and cost-effective for the patient and will clear the spider veins almost immediately.
Anti-inflammatories
• Sometimes, the physician may prescribe a combination of anticoagulants, anti-inflammatory drugs, and pain killers to suppress bulging of the affected blood vessels.
Prevention
Though there’s no guaranteed procedure of entirely preventing varicose veins, there are practices you can adopt to lower the risk of developing the condition. These practices include:
• Regular body exercise with more emphasis on lower body workouts.
• Maintaining a healthy weight.
• Consuming foods rich in fiber and low in sodium.
• Avoid wearing high heels and tight clothing.
• Adjusting your standing and sitting positions regularly.

